Artificial Intelligence (AI) has been steadily transitioning from science fiction into being an integral part of many people’s every day lives, including healthcare practitioners. From the initial experimental algorithms through to the widespread deployment in clinical and operational settings, AI’s role in medicine has significantly expanded in the past few years. Today, healthcare providers are increasingly reliant on sophisticated AI tools to improve diagnostic accuracy of diseases, streamline administrative processes, and personalize treatments. Each of these is having profound impacts on patient care.
This rapid evolution of AI in healthcare settings is fueled by the unprecedented growth in large scale data, computational power, and advancements in machine learning techniques. Models previously relegated to the realm of the theoretical are now being used to actively interpret medical images like MRI, forecasting patient risks or better treatment options, and managing healthcare operations efficiently. Even autonomous AI assisted robots are assisting in surgical procedures. Much of this rests in AI’s capability to analyze truly massive datasets of genomic and clinical data, allowing for breakthroughs in personalized medicine down the road.
Like most scientific advancement, adoption of these tools comes with complex challenges. Issues surrounding data privacy, inherent biases within algorithms, and regulatory frameworks that lag behind the rapid advances in the field require attention and pragmatism going forward. The integration of AI into healthcare aims to be ethical, equitable and patient focused, things that are critical to building public trust and to its long term success.
Here I will look at the current state of AI in healthcare. I’ll highlight further opportunities for further integration while discussing the challenges and ethical considerations that must be taken into account.
Current Applications of AI in Healthcare
Diagnostics and Medical Imaging
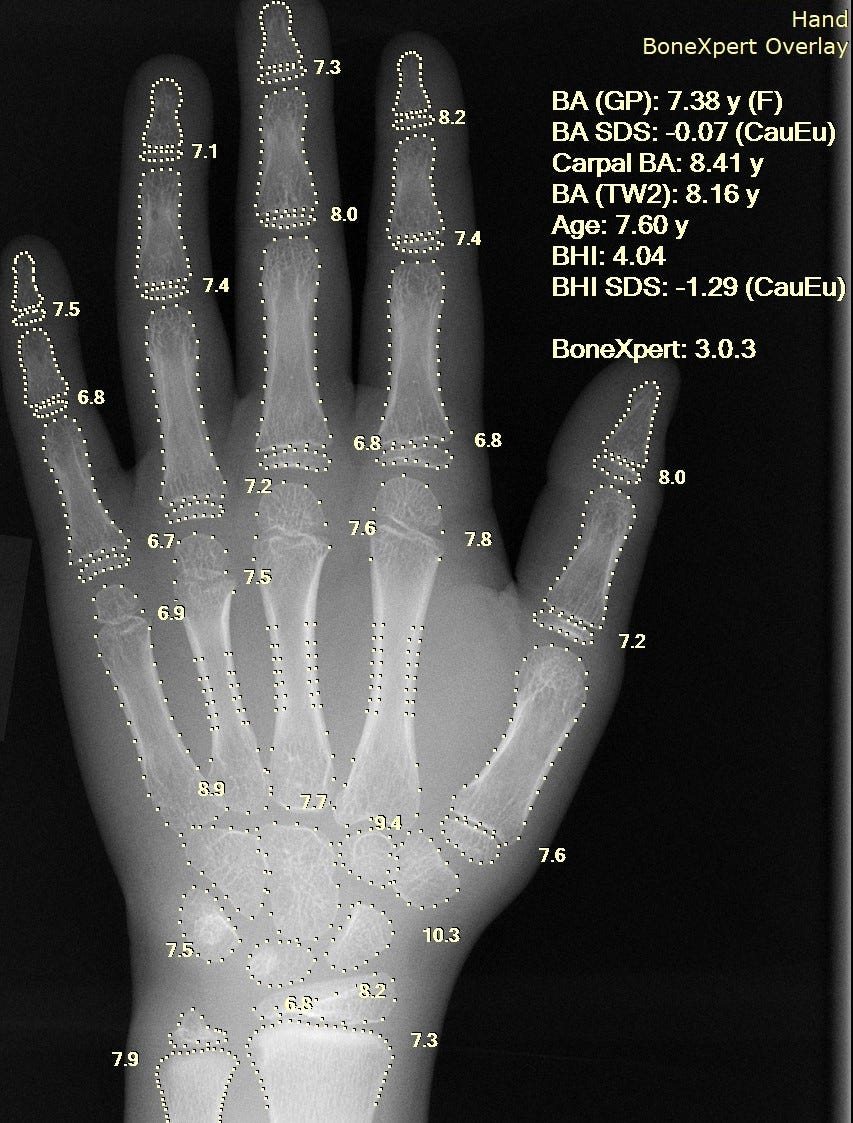
AI -based tech has dramatically transformed the diagnostic and medical imaging practices. Radiologists and pathologists have worked with advanced machine learning algorithms to significantly enhance accuracy and efficiency in interpreting medical images for a decade (X-rays, MRIs, pathology slides, etc.) [1, 2]. These tools already enable providers to detect early stages of diseases like cancer with much higher accuracy. For instance, in 2017 algorithms were already identifying gastric cancer related RNA markers [8] and deep neural networks were classifying skin cancer at the same level of accuracy as a dermatologist [9], showcasing the role of AI in diagnostics. More recently, research has highlighted the ability to use AI to analyze wearable device data and predict outcomes from Electronic Medical Records. This dramatically enhances diagnostic capabilities and its potential for preventive care, as these usually have massive datasets that can be incredibly complex and time consuming to analyze without these techniques [17].
Treatment Personalization
Personalized medicine has also benefited from integration with AI. AI tech uses natural language processing to effectively extract and analyze phenotypic features from the medical literature, allowing for quicker identification of congenital abnormalities and rare diseases [10]. The analysis of genomic and clinical data has also been streamlined with AI, allowing for more tailored treatments to individual patients. This helps to optimize therapeutic outcomes and reduce adverse effects [6, 7]. The comprehensive approach allowed by AI helps to identify molecular targets for medications, leading to new drug discoveries and allowing for better treatment selection and quicker clinical trial design via the innovation of “digital twins” [17]. Digital twins are AI driven virtual models of patients that simulate physiological and clinical outcomes. Genomic data, medical imagine, EHR, and wearable sensor data create a digital replica of the patient. While still in the early stages, this represents a major leap forward toward hyper personalized medicine.
Administrative and Operational Efficiency
Ai applications extend beyond the clinical practice and into administrative and operational areas, helping to enhance efficiency and reduce operational costs. Predictive analytics and automated administrative tasks smooth out hospital operations like patient scheduling and billing [4]. Improvements like this increase patient satisfaction through the reduction of wait times and allowing healthcare providers to allocate resouces more effectively [11]. There is also the potential to transform healthcare in low and middle income countries by improving access, reducing costs, and becoming more efficient in the same ways previously mentioned. Challenges like resource constraints, bias mitigation, and other ethical considerations will need to advance with the technology. This means collaboration across sectors to ensure equitable, responsible AI deployment [17].
Future Prospects of AI in Healthcare
Most of what I have covered so far are the more well established aspects of AI in healthcare (thus the older sources). It’s difficult to predict where AI might go from here, but I’m going to do my best as an outsider who casually uses AI for work and in general. I’ve seen how fast this field has moved and would honestly not be shocked by many features to come in the future simply because it seems like the sky truly is the limit here.
Enhanced and Multimodal Diagnostics
The future prospects for AI in healthcare have to include enhanced multimodal, multi-omic diagnostics. This would consist of multiple data streams being combined (imaging, genomic, clinical data, microbiome, etc) to substantially improve precision diagnostics and prognoses by enabling a more full view of the patient’s health. Leveraging advanced algorithms should allow for the detection of the early stages of diseases like Alzheimer’s and allow for better prediction of the trajectory symptoms will be one.
Robotics and Surgical Innovations
The surgical systems used in surgery will become increasingly more sophisticated, making the transition from supervised to more autonomous operations. Advanced systems will be able to execute complex procedures with precision rivaling the best human surgeons in history, with less invasiveness, and reduced recovery times. There is ongoing development of semi-autonomous and fully autonomous surgery systems representing a huge shift in surgical practice with the potential to expand access to specialized surgeries even in more remote, underserved areas.
Patient Engagement and Remote Monitoring
AI should have the power to empower patients through more personalized health monitoring systems and tools. Wearables are slowly making their way into the mainstream in the form of watches, rings, and continuous glucose monitors. These wearables when enhanced by AI will be proactive health managers for chronic illnesses, providing real time feedback to help with adherence to treatment regimens.
Challenges and Ethical Considerations
Data Privacy, Security, and Patient Trust
With AI systems further integrating into healthcare, concerns about data privacy and security become more and more urgent to address. AI models rely on massive datasets, including sensitive patient information to train and improve their algorithms. Making sure that these datasets stay secure and that patient confidentiality is not broken is a serious challenges. Healthcare systems in the past have had data breaches, unauthorized access, and patient record misuse, all of which could be exacerbated by the incorrect use of AI or by bad actors.
Healthcare institutions will need to implement robust encryption techniques, employ strict data access controls, and have fully transparent AI governance policies that prioritize patient rights. Emerging regulations on AI will likely include more strict compliance measures with regard to data sharing and anonymization to keep patient trust.
Bias and Fairness in the Algorithm
If AI systems are trained on non-representative data, they may come up with inaccurate results for populations with a lower level of representation in the data, leading to misdiagnosis or ineffective treatment. So despite AI having the potential to improve healthcare, disparities could be created without careful selection of the data that these models are trained on.
Regulator and Legal Challenges
AI has advanced so quickly it has outpaced the existing regulatory frameworks. This creates uncertainty around the approval processes, liability, and ethical guidelines. Regulatory bodies like the FDA, EMA, and WHO are working to establish guidelines for AI healthcare tools, but there are challenges in ensuring these regulations are able to keep up with the technological advancement of the field. Some of the key issues include:
Liability questions: who is responsible for an incorrect AI derived diagnosis?
Transparency: should AI decisions be explainable and how much information can realistically be disclosed to patients with the expectation that they understand how the decision was made?
Informed consent: how do we make sure patients understand and agree to AI-based medical decision making?
These ethical considerations are going to remain at the forefront of AI regulation. Unclear regulations and guidelines increase the risk of unintended harm, legal dispute, and degradation of public trust in AI as a technology [14, 16].
The Road Ahead
As AI evolves, the impact on healthcare will only get larger. The potential for AI to enhance all different aspects of medicine from diagnostics to administration is hard to deny. But achieving this level of promise will require proactive governance with the right amount of oversight.
Looking ahead, some key priorities to gain more public trust should include closing data gaps and ensuring transparency of models so they are explainable to a non-AI researcher, along with balancing innovation with safety. This calls for a collaborative effort of policymakers, doctors, the engineers, and patients to create AI driven solutions that are effective and ethical.
This is not just about efficiency or automation, its about enhancing decision making with regard to medical questions and expanding access to quality care. Some of the greatest benefits will come from AI systems that support clinicians, not ones that replace them. Ultimately the future of AI in healthcare doesn’t just hinge on further advancements. It hinges on how responsibly we choose to implement them. We have a promising path forward, but we need to navigate it with care.
References
1. Jiang, F., Wang, L., Zhang, Y., et al. (2017). Artificial intelligence in healthcare: Past, present, and future. Stroke and Vascular Neurology, 2(4), 230-243.
2. Jha, S., & Topol, E. J. (2016). Adapting to artificial intelligence: Radiologists and pathologists as information specialists. JAMA, 316(22), 2353-2354.
3. Rajkomar, A., Oren, E., Chen, K., et al. (2018). Scalable and accurate deep learning with electronic health records. npj Digital Medicine, 1, 18.
4. Davenport, T., & Kalakota, R. (2019). The potential for artificial intelligence in healthcare. Future Healthcare Journal, 6(2), 94-98.
5. Shademan, A., Decker, R. S., Opfermann, J. D., et al. (2016). Supervised autonomous robotic soft tissue surgery. Science Translational Medicine, 8(337), 337ra64.
6. Topol, E. J. (2019). High-performance medicine: The convergence of human and artificial intelligence. Nature Medicine, 25(1), 44-56.
7. Mesko, B. (2017). The role of artificial intelligence in precision medicine. Expert Review of Precision Medicine and Drug Development, 2(5), 239-241.
8. Li, J., Chen, X., Li, X., et al. (2017). Identifying novel gastric cancer-related long non-coding RNAs by integrating genomics data from GEO and TCGA. Scientific Reports, 7, 44715.
9. Esteva, A., Kuprel, B., Novoa, R. A., et al. (2017). Dermatologist-level classification of skin cancer with deep neural networks. Nature, 542(7639), 115-118.
10. Karakülah, G., Dicle, O., Koşaner, Ö., et al. (2014). Computer-based extraction of phenotypic features of human congenital anomalies from the digital literature with natural language processing techniques. Studies in Health Technology and Informatics, 205, 570-574.
11. Reddy, S., Fox, J., & Purohit, M. P. (2019). Artificial intelligence-enabled healthcare delivery. Journal of the Royal Society of Medicine, 112(1), 22-28.
12. Price, W. N., & Cohen, I. G. (2019). Privacy in the age of medical big data. Nature Medicine, 25(1), 37-43.
13. Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S. (2019). Dissecting racial bias in an algorithm used to manage the health of populations. Science, 366(6464), 447-453.
14. Gerke, S., Minssen, T., & Cohen, G. (2020). Ethical and legal challenges of artificial intelligence-driven healthcare. Artificial Intelligence in Healthcare, 295-336.
15. He, J., Baxter, S. L., Xu, J., et al. (2019). The practical implementation of artificial intelligence technologies in medicine. Nature Medicine, 25(1), 30-36.
16. Char, D. S., Shah, N. H., & Magnus, D. (2018). Implementing machine learning in healthcare—Addressing ethical challenges. New England Journal of Medicine, 378(11), 981-983.
17. Nature Medicine. (2025). Various AI applications in healthcare. Retrieved from nature.com.




IBMs Watson was a Tinkertoy compared to today’s AI. Decade too soon but did explore the area pretty nicely particularly in the imaging diagnostic area with their purchase of Merge who had petabytes of training data from their business model. What’s happening today will be amazing but I am curious where they get their training data :)