How to Kill a Cancer Vaccine: RFK Jr. and the Campaign to Undermine One of Public Health’s Greatest Wins
If you wanted to design the perfect vaccine, it might look a lot like the one for HPV.
It prevents infection with a virus that causes cancer. It works best when given before exposure, ideally in adolescence, and it’s one of the few interventions in all of medicine that can directly prevent multiple kinds of cancer in one go. Cervical, anal, oropharyngeal, vaginal, and penile. It’s a rare, genuine win in public health.
And yet, if you spend even a few minutes in certain corners of the internet, or unfortunately, the U.S. Government, you’d think it’s poison.
Robert F. Kennedy Jr. has been on a crusade against vaccines for years, but HPV holds a special place in the anti-vaxx rhetorical canon. It involves kids. It touches sex. And it’s wrapped in just enough plausible-sounding biochemistry and moral panic to convince the skeptical that they’re being cautious rather than conned.
This post is for anyone who’s heard those arguments and wondered if there’s something to them. It’s not for the die-hard grifters, it’s for the people caught in their blast radius. Parents who want to do right by their kids. Readers who’ve been burned before by pharma. People who still believe evidence matters. Because the evidence about HPV vaccines is overwhelming.
This is a vaccine that prevents cancer. And the only thing more dangerous than ignoring that fact is allowing people like RFK Jr. to muddy the waters around it.
Let’s walk through the myths and the reality of one of public health’s greatest accomplishments.
Myth #1: “HPV Isn’t That Dangerous”
This is where the misinformation usually starts. If HPV is common and often clears on its own, why treat it like a medical emergency?
HPV (human papillomavirus) is the most common sexually transmitted infection in the world. Nearly every sexually active person will encounter it at some point. Most infections are harmless and go away on their own. But the strains that don’t, especially HPV 16 and 18, are directly responsible for:
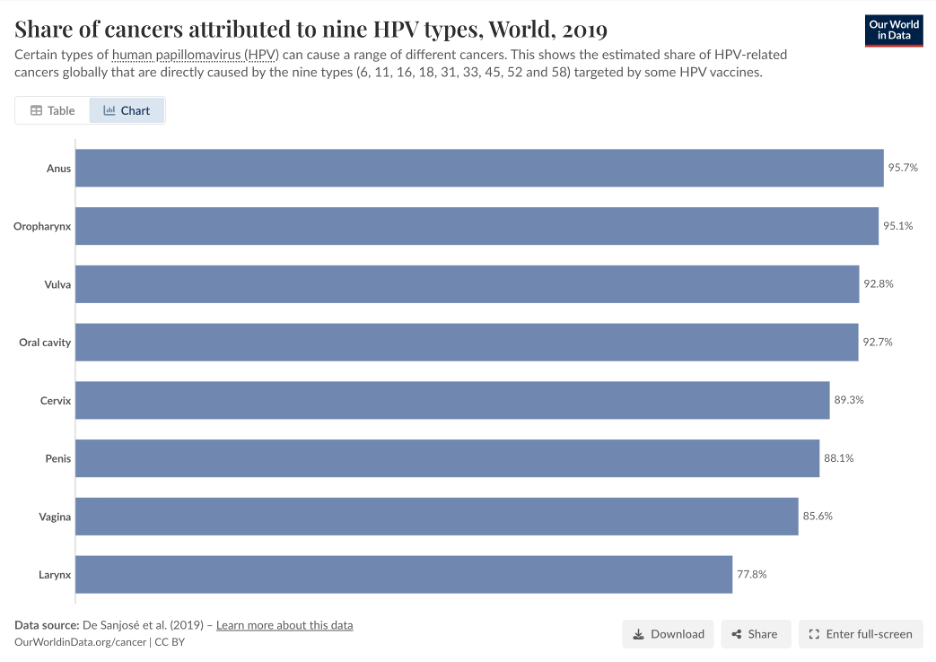
Over 90% of cervical cancer cases1
The majority of anal, vulvar, vaginal, penile, and oropharyngeal cancers1
An estimated 690,000 cancer cases per year globally1
In the U.S., cervical cancer alone kills over 4,000 women annually2. Globally, that number is over 340,0003, with the vast majority in countries with limited access to screening.
And these are slow-growing cancers, which helps with treatment options, but that doesn’t make them benign. The slowness just makes them easier to prevent. That’s what makes the vaccine so powerful.
RFK Jr. and others love to talk about “natural immunity.” But HPV doesn’t care how good your diet is. You don’t beat this type of cancer with clean living. You beat it with prevention. And that’s exactly what the vaccine does.
Myth #2: “Screening Is Enough”
This one sounds reasonable on its face. After all, we’ve made massive strides in cervical cancer prevention through routine Pap smears and HPV testing. Isn’t that enough?
Not even close.
Screening is only secondary prevention. It catches disease after you’ve been infected, in this case after abnormal cells have started to grow. It can save lives, yes. But it doesn’t prevent the infection in the first place, and it certainly doesn’t eliminate HPV from the population. And it can’t help with HPV-driven cancers that are harder to screen for, like oropharyngeal and anal cancers1.
In real-world terms, the difference between vaccination and screening is this:
Vaccination: Stops HPV before it infects tissue
Screening: Hopes to catch cellular damage early enough to intervene
And even in countries with decent screening infrastructure, we see late-stage disease. In the Indian study referenced earlier, five-year survival plummeted to 55%, with late-stage presentation still common3.
Worse still, men (who are not routinely screened) are increasingly affected by HPV-driven oropharyngeal cancers, now more common than cervical cancer in parts of North America1.
The best protection isn’t waiting to catch disease. It’s stopping it before it ever starts. That’s what vaccination offers and screening alone simply can’t do the job.
Myth #3: “We Don’t Know If It Works”
This one’s the easiest to refute, because we do know (as you’ve seen already).
We know because we’ve tracked millions of vaccinated people for more than a decade. We’ve studied them in clinical trials, national cancer registries, and real-world screening programs. And everywhere we look, the same pattern emerges: when more people get vaccinated, fewer people get cancer.
Here’s what the data actually show:
In Scotland, a 2024 cohort study followed nearly half a million women. Among those vaccinated at age 12–13, there were zero cases of cervical cancer by age 25. Zero. Not a single one4.
Women vaccinated later, ages 14–18, still saw a 73–78% reduction in cancer risk compared to unvaccinated peers. But the earlier the vaccine, the stronger the protection4.
In Sweden, girls vaccinated before age 17 had an 88% lower risk of developing cervical cancer5.
In the United States, cervical cancer incidence among women aged 15–24 fell 29% in the decade after the vaccine was introduced2. No other explanation fits the timing or slope of that decline.
In Slovenia, rates of high-grade precancerous lesions (CIN2+) were 42% lower in vaccinated women, even after adjusting for screening participation (Irzaldy et al., 2025).
And across multiple countries, meta-analyses have shown declines in HPV infection, genital warts, precancers, and cancer incidence, especially when vaccination is started early1.
This isn’t a maybe. It’s a fact. The HPV vaccine works.
And it works best when given before exposure, ideally around ages 11-13, before the virus has a chance to take hold. That’s not because anyone expects kids to be sexually active at that age. It’s because immunity takes time, and prevention only works when it comes before the thing you’re trying to prevent.
Myth #4: “It Encourages Teen Sex”
Let’s get this out of the way: this myth isn’t about science. It’s about control.
The claim goes like this: if you vaccinate kids against a sexually transmitted virus, they’ll take it as a green light to be sexually active. And so, the argument continues, giving them the HPV vaccine might cause them to have sex earlier, or have more partners, or be “reckless.”
It’s a fear-based argument. And it’s wrong.
What the Data Says:
A large U.S. insurance claims study followed over 200,000 girls and looked at rates of STIs before and after vaccination. The result?
No significant increase. Not in chlamydia, not in gonorrhea, not in anything else6.
A Canadian review of behavioral outcomes found the same across multiple studies:
No change in age of sexual debut, STI rates, or pregnancy7.
A study from Ontario even showed a decrease in teen pregnancies among vaccinated girls likely reflecting better healthcare access, not risky behavior8.
In short: this myth has been debunked across three countries and more than a decade of surveillance data. The people pushing it just don’t care.
And let’s be honest, if you believe this vaccine will “make your kids have sex,” the issue isn’t the vaccine. It’s your theory of parenting. The HPV vaccine doesn’t affect the values you instill in a child. It doesn’t cause or change behavior. It prevents cancer, plain and simple. Let’s stop pretending otherwise.
Myth #5: “The Vaccine Isn’t Safe”
If you spend enough time listening to RFK Jr. or those in his circle, you’ll hear the usual claims: that the HPV vaccine causes various autoimmune disease, infertility, seizures, or some vague catch-all phrase like “serious complications.”
These claims don’t come from real-world data. They come from VAERS anecdotes, cherry-picked case reports, and years of digging through rabbit holes. Meanwhile, here’s what actual pharmacovigilance says:
Real-World Safety Data:
· The HPV vaccine has been studied for over two decades and administered to hundreds of millions of people worldwide.
· A 2022 umbrella review of post-licensure surveillance and RCTs found no consistent evidence of serious adverse effects1
· The European Society of Gynaecological Oncology (ESGO) and WHO call HPV vaccination “one of the most thoroughly evaluated vaccine platforms ever” 1
· A U.S. safety review covering over 60 million doses found:
- No increased risk of autoimmune disease
- No signal for infertility or premature ovarian failure
- No uptick in seizure or syncope beyond what’s expected from adolescent needle anxiety2
And yet, RFK Jr. treats this like thalidomide 2.0. His Children’s Health Defense site has promoted articles falsely linking Gardasil to chronic illness, all without disclosing the massive body of contradictory evidence9.
Is the HPV vaccine risk-free? No, because no vaccine is. But the risks are tiny and transient: headache, fatigue, low-grade fever. The benefits? Cancer prevention for life. That’s a trade anyone reasonable would make.
Clear Evidence and Loud Lies
Let’s recap: the HPV vaccine prevents cancer. It’s safest and most effective when given early. It doesn’t make teens reckless. It doesn’t mess with fertility. And it’s been studied harder than almost any other vaccine on Earth. But you wouldn’t know that from listening to RFK Jr.
Instead, you’d hear vague allusions to “injuries,” to government conspiracies, to “the rise in chronic disease” as if vaccines caused the modern world. You’d hear the kind of confident pseudoscience that turns anecdotes into absolutes, mechanisms into mandates, and public health victories into imagined crimes.
And all of it, all of it, relies on you not checking. On you not reading the studies. On you not seeing the survival curves from Scotland, or the registry data from Sweden, or the fact that over 200,000 girls in Ontario got vaccinated and nothing changed, except that fewer of them got pregnant or got sick.
The people pushing this narrative aren’t confused. They’re committed to the grift. To their ideology. To a worldview where medicine is always suspect and only their brand of “truth” is pure.
But vaccines don’t care about that. Cancer doesn’t care about that. Your cervix, your throat, your child’s future, none of it cares how good someone is at going viral on Twitter.
What matters is what works. And this vaccine works.
So here’s the ask: fight the narrative. Not with condescension, but with clarity. Not with rage at parents who hesitate, but with outrage at those who profit off that fear. Share the numbers. Post the graphs. Be the calm one in the room who says, “Actually, we know exactly what this vaccine does. And it’s not what they’re telling you.”
If we get this right, we don’t just win an argument. We get to watch a generation grow up without ever facing the kind of cancer their parents feared. That’s worth fighting for.
Citations
1. Taumberger N, Joura EA, Arbyn M, Kyrgiou M, Sehouli J, Gultekin M. Myths and fake messages about human papillomavirus (HPV) vaccination: answers from the ESGO Prevention Committee. Int J Gynecol Cancer. 2022;32(10):1316-1320. doi:10.1136/ijgc-2022-003685
2. Guo F, Cofie LE, Berenson AB. Cervical Cancer Incidence in Young U.S. Females After Human Papillomavirus Vaccine Introduction. Am J Prev Med. 2018;55(2):197-204. doi:10.1016/j.amepre.2018.03.013
3. Yadav M, Kumar HS, Kumar R, Sharma N, Jakhar SL. Survival pattern in cervical cancer patients in North West India: A tertiary care center study. J Cancer Res Ther. 2022;18(6):1530-1536. doi:10.4103/jcrt.jcrt_342_21
4. Palmer TJ, Kavanagh K, Cuschieri K, et al. Invasive cervical cancer incidence following bivalent human papillomavirus vaccination: a population-based observational study of age at immunization, dose, and deprivation. JNCI J Natl Cancer Inst. 2024;116(6):857-865. doi:10.1093/jnci/djad263
5. HPV Vaccination and the Risk of Invasive Cervical Cancer | New England Journal of Medicine. Accessed April 24, 2025. https://www.nejm.org/doi/full/10.1056/NEJMoa1917338
6. Jena AB, Goldman DP, Seabury SA. Incidence of Sexually Transmitted Infections After Human Papillomavirus Vaccination Among Adolescent Females. JAMA Intern Med. 2015;175(4):617-623. doi:10.1001/jamainternmed.2014.7886
7. Donken R, Ogilvie GS, Bettinger JA, Sadarangani M, Goldman RD. Effect of human papillomavirus vaccination on sexual behaviour among young females. Can Fam Physician. 2018;64(7):509-513.
8. Smith LM, Kaufman JS, Strumpf EC, Lévesque LE. Effect of human papillomavirus (HPV) vaccination on clinical indicators of sexual behaviour among adolescent girls: the Ontario Grade 8 HPV Vaccine Cohort Study. CMAJ. 2015;187(2):E74-E81. doi:10.1503/cmaj.140900
9. HPV - Gardasil Archives. Children’s Health Defense. Accessed April 24, 2025. https://childrenshealthdefense.org/research_category/hpv-gardasil/